About the Project
Delirium or acute confusional state , is an organically caused decline from a previously attained baseline level of cognitive function. This was a 48 hr design challenge at University of Pennsylvania along with students from Northwestern University , Massachusetts Institute of technology and Carnegie Mellon University in collaboration with UPENN college of medicine that organized the annual integrated innovation challenge.
Project Brief : How can caregivers be enlisted to mitigate delirium / post operative cognitive dysfunction and expedite recovery when the patient demonstrates symptoms of delirium post surgery in the hospital
Team : Nicholas Philiphs -Northwestern University , Masakazu Nagata - MIT , Madeleine Klichowski - Northwestern University,
Danielle Lashley - University of Pennsylvania
Role : Research , Concept Prototyping
Duration : 48 Hour Design Challenge
DAY 1 :
what is delirium
The design & innovation challenge began with Dr. Sushila ( Professor of Anesthesiology at Penn Medicine ) briefing the cross disciplinary teams on what delirium is ,how it affects patients post surgery and their behaviors when affected with delirium. Teams were divided to tackle various stages of delirium over the course of 48 hours.
guerrilla research
The team started reviewing audio and video transcripts of nurses and patients suffering from Delirium.
INSIGHTS :
The team found some common trends after reviewing the transcripts
POCD patients suffer from mild to intense hallucinations
Delirium can last from 48 hrs to 14 days post surgery
Cognition and memory association skills are affected
The families of the patients feel unprepared
Day 2
expert interviews
Research was conducted with primary caregivers, family members of patients, ethnographers , physicians and doctors currently related to post operative cognitive disorder.
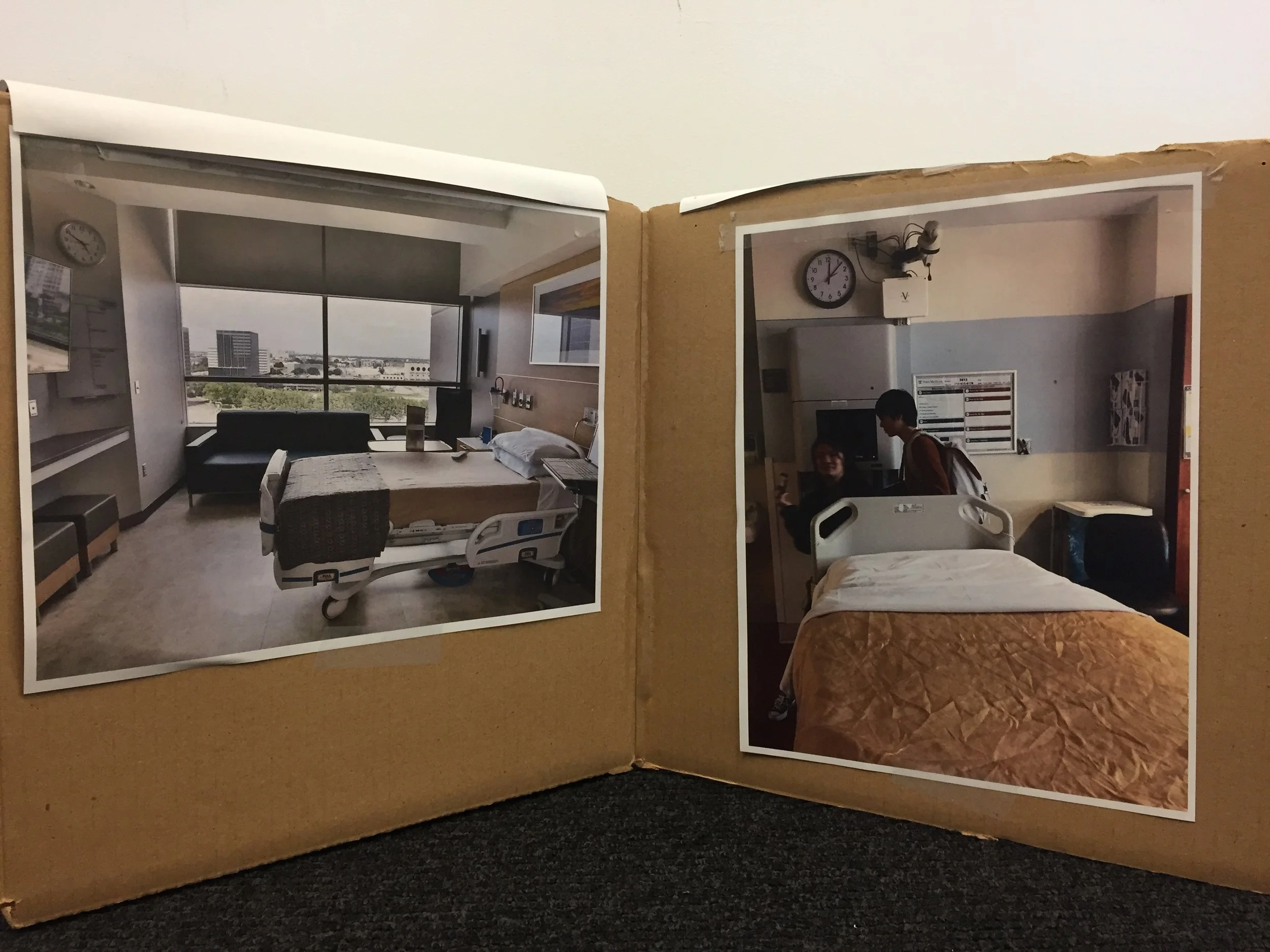
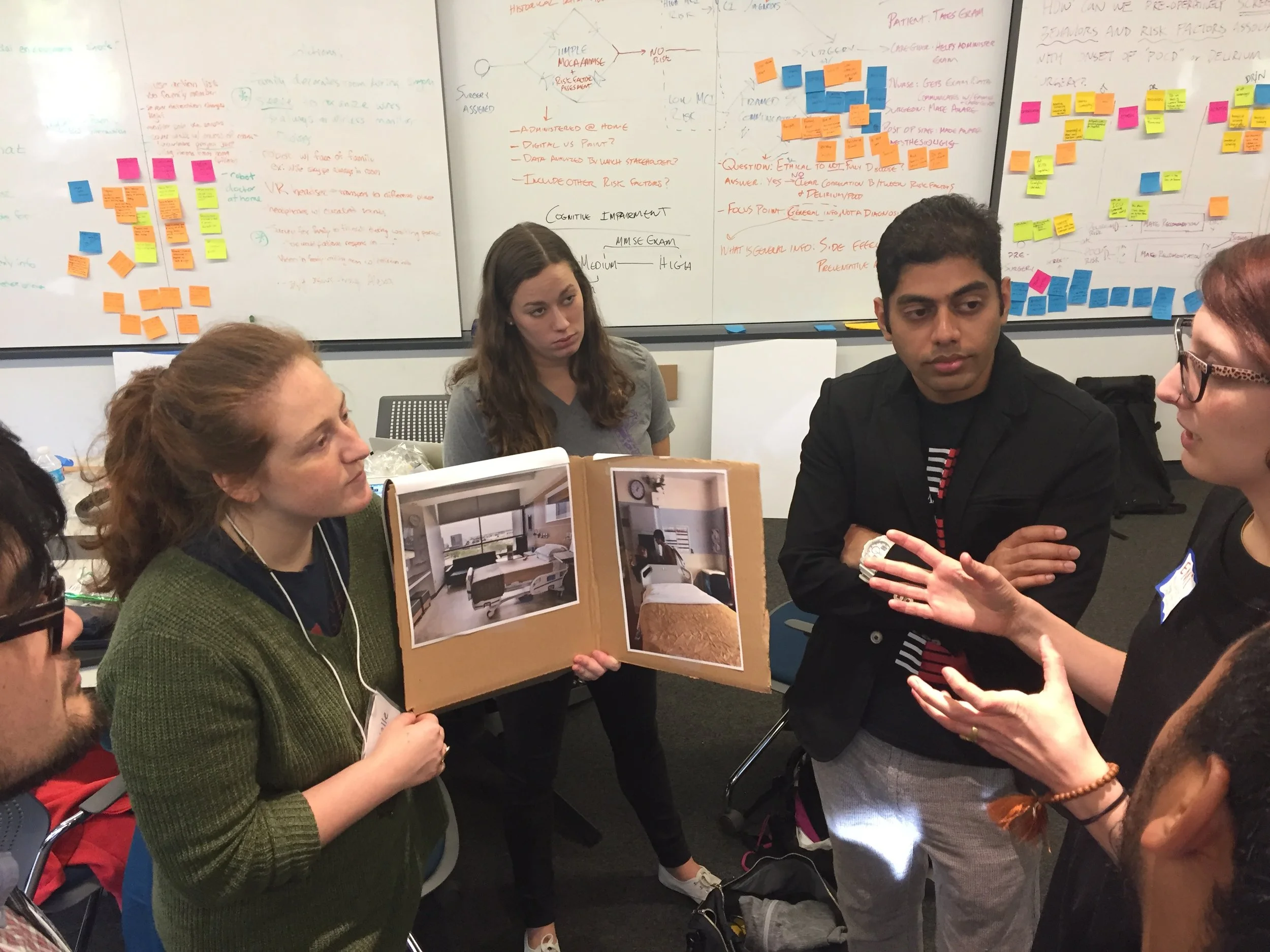
SPEED DATING EXERCISE WITH PRIMARY CAREGIVERS AND FAMILY MEMBERS
As part of the speed dating exercise we asked the primary caregivers and the patient to walk us through a particular POCD episode / scenario they had been in . Based on their feedback , we placed ourselves in their position and experienced a glimpse of what it feels like to wake up in an unfamiliar hospital room and experience delirious sensations.
INSIGHTS :
Caregivers panic when they see patients showing symptoms of delirium and might worsen the situation for the patient
The environment around the patients plays a major role in amplifying the effects of delirium such as light, sound and movements
Patients did not recognize their families
The primary caregiver had to step up and take care of the situation
INTERVIEW SESSIONS WITH ANTHROPOLOGISTS AND RESEARCHERS FROM UPENN MEDICINE
INSIGHTS :
Pre surgery meeting between the patient and the surgeon is very brief and does not talk about the risk of the surgery
Patients are not prepared in advance for this procedure
Surgeons have meetings with 40 patients in 6 hours
DIRECTED STORYTELLING WITH DOCTORS AND PRACTICING PHYSICIANS
INSIGHTS :
Patients are allowed some personal belongings with they are attached with
Patients are nervous before the surgery
Family members are not allowed into the post surgery recovery room or at least two hours
PROBLEM FRAMING
How might we reduce the fear of the unknown within the first few minutes of waking up in the post-op room ?
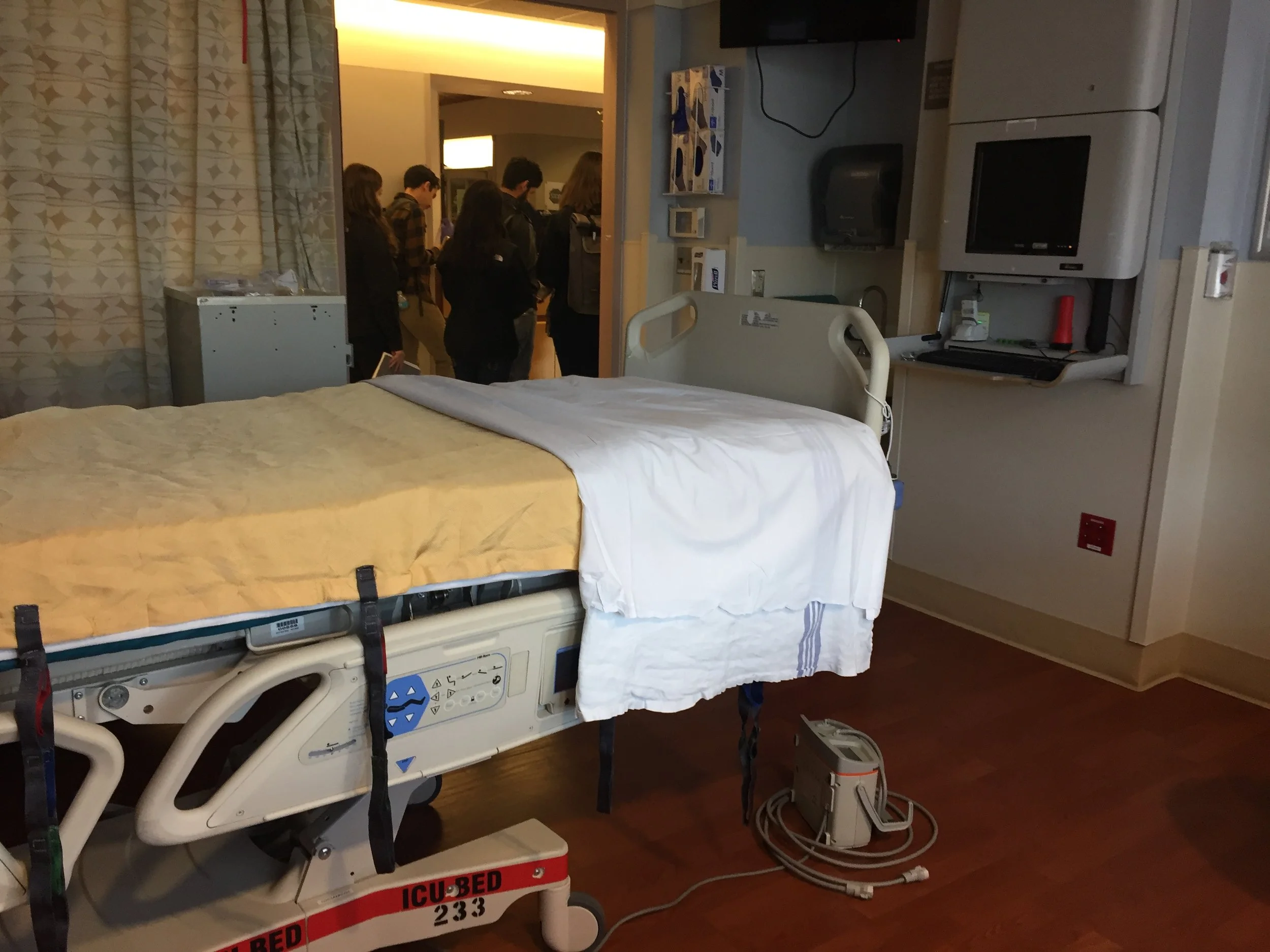
VISITING PENN MEDICINE CARE HOSPITAL : CONTEXTUAL INQUIRIES
INSIGHTS AND KEY FINDINGS
Family members fell unprepared as there are no existing protocols if patients demonstrate symptoms of Delirium
In most cased patients experience delirium immediately post surgery when they are by themselves
Patients wake up to an unfamiliar environment post surgery
Patients suffer from hallucinations and feel separated from reality.
REFRAMING THE PROBLEM
How might we introduce familiar memories to reduce the fear of the unknown within the first few minutes of waking up in the post-op room?
finding common trends from our insights
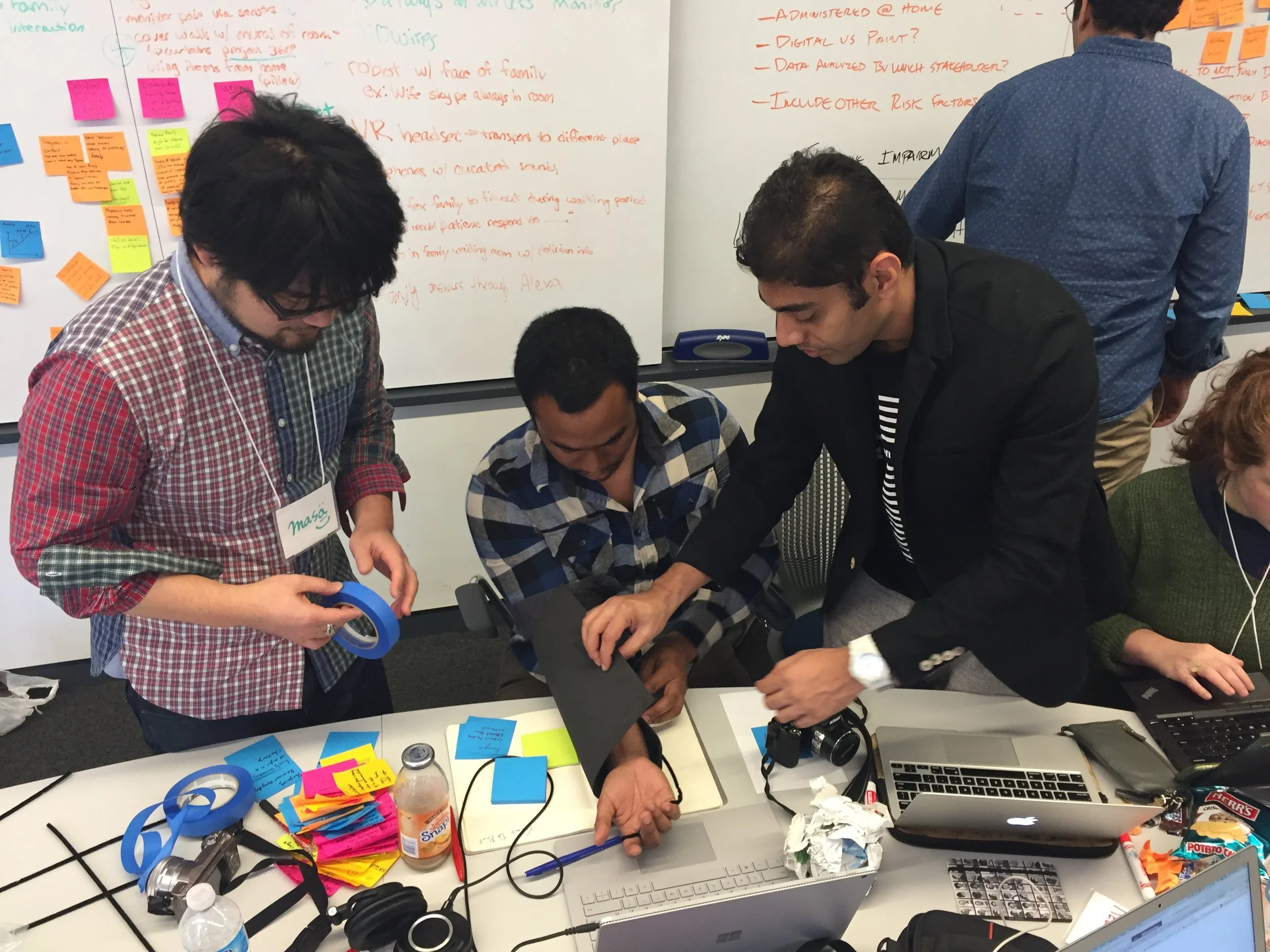
Prototyping solutions
The team prototyped 3 solutions .
1) A wearable arm jacket equipped with sensors to inform how the patient is feeling ,
2) A 360° projection of one's home on the walls of the hospital room to make the atmosphere familiar
3) A video kiosk where families can learn about delirium and leave a message for their loved one .
FEEDBACK FROM DOCTORS
Feedback from Doctors and experts gave us insights on the feasibility, deployability in hospitals and impact the solution would have . This helped us narrow down the solution to providing the service of educating family members on delirium and create a video message for the patient which would help them make memory associations.
OUR FINAL SOLUTION
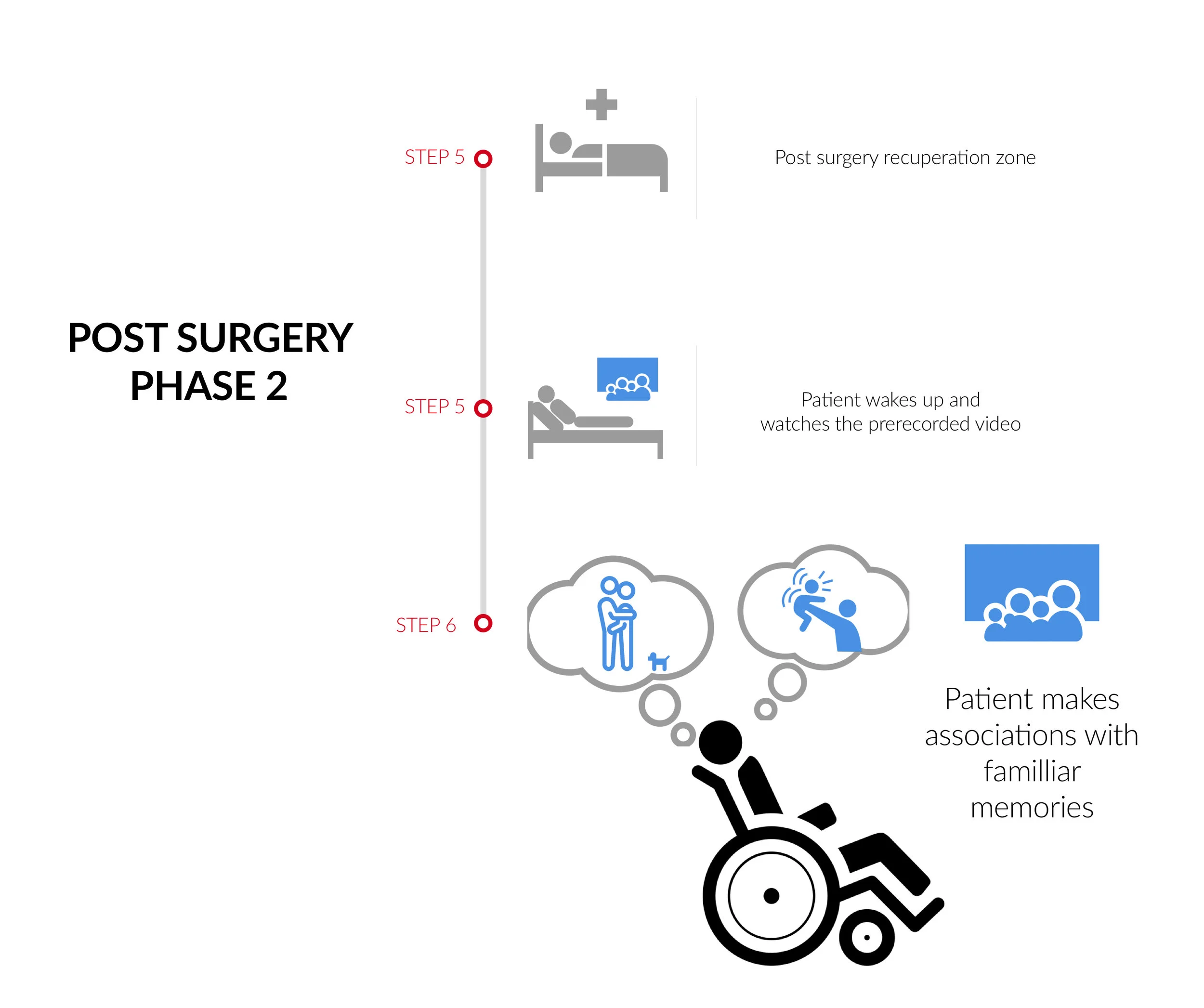
As a team we suggested a service for the primary caregivers, families and the patients :
Goals of the Solution :
To inform primary care givers what delirium is.
To assist the patient in making memory associations post surgery.
solution timeline
WHAT WE ACHIEVED
As an interdisciplinary team we had the opportunity to observe and learn different methodologies to innovate solutions for patients suffering from post operative cognitive dysfunction. The best part of the challenge was inter university collaboration which resulted in the team using different research and analytical methods to solve problems and innovate lo fidelity solutions in 48 hours.